Note: If you haven’t read Processing Birth: Part 1, you might find yourself a bit lost here. I would suggest reading that first.
When I felt my body start to push, I was in shock. I had experienced the spontaneous urge to push with Emmett, but I had labored for many hours at that point with him, so this next step made sense. With Baker, however, I hadn’t even been certain I was in labor for real until an hour or so before this moment. When I told the nurse I had no breaks between contractions, I knew I would be able to skip triage, not skip every step in the process altogether and practically deliver this baby in the hallway.
I was asked if I wanted a wheelchair but I declined, having no idea how I would sit down in that moment. We stepped out into the hallway and the nurse told us to go to the right; “we are going to take you straight to L&D, no need for triage at this point.” We had taken maybe 1 step to the right when I had to stop for a contraction and started to feel the urge to push. The nurse immediately rerouted us to the left and towards the nearest room. Someone helped me kneel onto a wheelchair and I was whisked down the hall whilst pushing.
By this point in my career as an avid birth nerd, I knew how to advocate for myself. But at this moment, did I really need to? I have no idea what came out of my mouth and what simply happened inside my head, but when I said “I am pushing” and abruptly threw myself onto the bed the moment it was within my reach, I would assume I might be taken seriously? Nope.
At 5:07am I managed to climb onto a bed on all fours and someone turned on a monitor (which is the only reason we know the timing). I haven’t the faintest idea who was in the room at this point but I felt like no one was listening to me, or maybe I wasn’t speaking. I vaguely heard discussion of trying to get me to flip over onto my back, but my sweet husband countered “she delivered our last one on all fours, she isn’t moving.” Good man, that one.
In this precise moment, between walking into the hospital at 4:53AM and climbing onto the bed at 5:07AM, I went from feeling completely incompetent and incapable in MY body, to feeling surrounded by incompetence and incapability. If you had asked me to do a line up (think police station, suspect identification) even moments after birth of the people in that room, I would not have recognized a single one. Not only did I not have time to look at them, but in the moments that followed, they did not feel worthy of my gaze. The exception to this is my midwife, Jenny (the same Jenny who delivered our second baby), who arrived just after the baby was out and eventually helped me deliver the placenta.
At one point I heard someone say “let me know when there’s a break so I can check you” and I’m sure if I had been coherent enough I would have laughed out loud. I frantically asked my husband to take my pants off when it became clear no one else was going to, and I believe someone must have reached down to check me as I said “I feel his head” because someone responded with “oh yea there’s a head!”
When Emmett was born, he was placed on my chest the moment I was able to flip over and lay down (having delivered on all fours). I can remember vividly how special this was, and how special it continued to be as he was never taken from me. Our daughter, Evelyn–my first birth–went to the NICU for 4 hours, but even she spent a few minutes on my chest before she was taken. With Baker, it was different.
I was still on all fours as I heard my husband ask to delay cord clamping, to which someone responded “I already clamped it, we need to cut.” Someone else spoke to me directly and said they needed to take baby away since he wasn’t breathing well. At some point during these moments my midwife got there, because I remember her showing up by my side. I told my husband to go with the baby as my midwife, Jenny, helped me flip over onto my back. By the time I was laying down, baby was in the next room and out of my sight.
I know the room I delivered in wasn’t ideal. It was a triage room, not meant for delivery, not meant for a baby. I know the staff did the best they could with what they were given, with safety as the top priority. There’s a good chance they couldn’t pick me out of a line up either. We didn’t know each other, we weren’t given time for introductions. But I do believe someone could have stepped back for a moment and taken in the gravity of the situation, seen the room for what it was, seen me for who I was and what I had just been through, and done things differently.
When you give birth to a baby, you also give birth to a whole lot of other goodies. Everyone knows about the magical placenta and the fear of poop escaping whilst pushing out the baby, but there’s also amniotic fluid, blood, uterine lining, just a whole puddle of baby-making goodness. When you give birth in a hospital, they usually “break down the bed” before you deliver; part of the bottom of the hospital bed comes away and they prep the room with methods for quickly disposing of everything that isn’t your sweet babe when it comes out. When you give birth at home, your bed gets plastic sheets, your birth tub gets a liner. The stage is set, the mess is handled preemptively, it becomes almost invisible in your birth.
When you give birth quickly, with absolutely zero prep time, the only priority–rightfully so–is catching the baby. The rest of the mess is dealt with later, the literal aftershocks of birth. So when Baker made his untimely entrance into the world on a normal, non-prepped bed, I was left sitting in a puddle of all that was previously inside of my body. I can vividly recall the feeling of each part of his body exiting mine… head, shoulders, arms, tummy, legs, feet… all of it. And then he was gone, whisked away before I could even flip over. While she didn’t catch the baby, Jenny, my midwife, appeared moments later, and it was her arms that helped me turn over and settle onto my back.

The triage room I delivered in had just enough space for a bed and a chair. Opposite the bed was a small hallway leading into an adjoining room, presumably mirroring my own. Between the rooms, there was a bathroom (well, a toilet behind a door). As soon as Baker came out, he was rushed through the hallway and into the other room, out of my sight. Andrew, my husband, went with him, and it was only his face I could see popping back through the hallway to assure me he was okay. I don’t recall anyone on baby’s team speaking to me while they worked or afterward. I know I told Andrew to go with him when they left for the NICU, but I’m not sure anyone actually talked to me. And then I was alone.
My midwife popped out to find supplies, and with no nurse actually assigned to me, it was a few minutes before anyone realized I needed tending to. I sat there, in a literal puddle, placenta yet to be delivered, numb. I was numb. After Emmett’s birth, which had also been unexpectedly quick and drug-free, I was in shock, my body shaking uncontrollably as I clung to the baby on my chest. With Baker, I was numb.
I know that Jenny returned with supplies and I delivered the placenta. I don’t remember any pain. Nurses popped in and out of my room, reeling in this high from my birth, the high I was supposed to feel. There was so much excitement, a baby delivered in triage, barely caught, on all fours no less. It was thrilling for them. One nurse even told me later, “he was just looking up at me, his face in that sack, like please catch me!” Through their recounts of my own story, I would learn that most of these nurses had never seen a doctor allow someone to give birth on all fours. Many women feel this high after drug-free birth, empowered by what their bodies have done, but I didn’t. A shell of myself, I laughed along with the nurses as they reminisced like this hadn’t just happened moments ago, taking pride in their participation in such a birth.
Jenny got down on her hands and knees to mop up some of the mess beneath the bed, presumably so no one would slip and fall before the room could be properly cleaned. I can remember apologizing to her… why was she on the floor? That wasn’t her job, she wasn’t meant to do that. A very chatty nurse stood at the monitor and asked me all of the questions that would usually have happened at check in. We went back and forth about whether I delivered at 5:10AM or 5:12AM, discussed how lucky we were that someone thought to turn on the monitor when we entered the room so we at least have a start time of 5:07AM.
At some point I was helped to the bathroom, though I think I insisted they leave me at the door because physically I felt no weakness. When I came back and looked at the bed, it was a massacre. I was ushered into the chair in the corner, with a pad beneath my bum, while the bed was stripped. I assumed someone would remake it… you’re always in bed after birth… but no one ever did. So I sat in that chair as everyone finished up their tasks and left. Jenny made me an electrolyte drink and then off she went, called to another birth. Alone again.
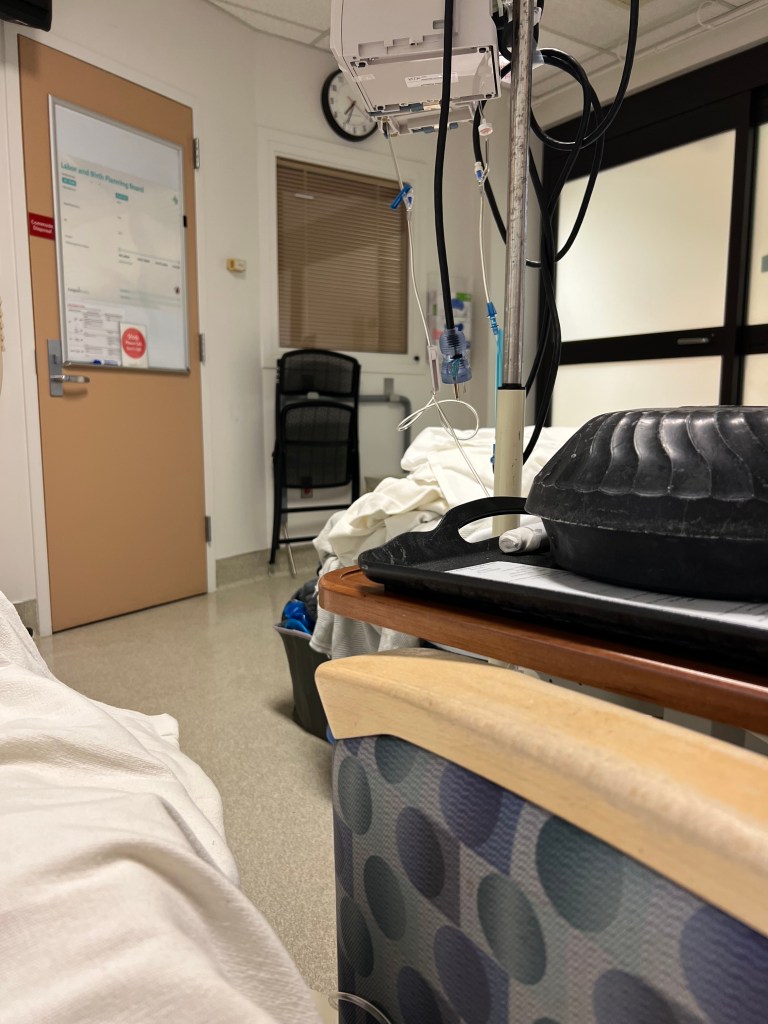
Andrew text me from the NICU, photos of our sweet baby. I assume I was uncomfortable, stuck as I was in a hospital chair (why are all hospital chairs so terrible), but the only memory that sticks with me is emptiness. After I had Evelyn, she spent four hours in the NICU. I was alone then too, but I had held her, looked at her, witnessed her before she went away. And it was 10PM then; in my exhaustion, I went to sleep. This time, however, not only was it bright and early in the morning, but I was in a chair, not a bed, so I couldn’t have slept if I had wanted to.

Baker was born at 5:12AM. We have a photo of me finally holding him at 9:22AM. I would spend the rest of that hospital stay in absolute awe of my perfect baby, while also fighting the system to let us leave as soon as humanly possible. It was June 2022, we were still dealing with the pandemic. We had no visitors, no reason to stay. I wanted to get home to my other kids, to reunite my family, to feel whole.
Baker is two years old now and he and I are attached. We are still breastfeeding and I cannot imagine cutting him off. I love all of my kids with every ounce of my being, but being apart from Baker makes my blood boil, my skin crawl. I feel physically uncomfortable, like this is all wrong. I ache for my other children when we are apart, but this primal sense of attachment is for Baker alone. I don’t love him more, he isn’t more important to me, but he was taken from me once, out of my sight once, and it broke me in a way that I haven’t quite figured out how to fix.


One thought on “Processing Birth: Part 2”