Note: I started writing this while still in the hospital, and I am finishing it at home. However, I chose to leave the notes I made whilst writing in the hospital, so if timing feels a tad inconsistent, bear with me. While I am writing this to share what happened, I am more-so writing it for me. I never want to forget the ins and outs of this.
When you’re on your third kid, there aren’t all that many firsts left. The first time you leave them with someone else, the first cold bug, the first lost tooth, the first scraped knee. By the third kid, there are few surprises left, few things yet to have experienced. Or at least that’s how it feels.
Until it doesn’t.
On March 1st, our sweet 3rd kiddo, our little baby boy, was admitted to the Children’s Hospital. This was a BIG first for us. It IS a big first for us… as I type this, I have this sweet babe strapped to my chest (THANK YOU, Hope & Plum Lark carrier, the best) while we wait for an IV expert to attempt a line for the second time tonight. Don’t get me wrong, we’re Urgent Care pros at this point. But the Emergency Room? No way. That’s hard core, that’s the big time, that’s “never going to happen to our kids.”
February is a busy month for us; Valentine’s Day, my birthday, middle kiddo’s birthday, it’s a lot. When illness struck during the last week of the month, it honestly wasn’t all that surprising. We’d been busy, we’d been social, and in this “post-pandemic” world, that’s risky business. Elementary school kiddo got hit first, and from there, between the coughing and the random vomiting from our vomit-prone middle kiddo (sorry, Emmett!), honestly it’s a bit of a blur. At some point, it became clear that while everyone else in the home was improving (or at least at a manageable baseline), sweet little baby Baker was not.
Let’s reflect on the timeline for a moment… By 2/24, every member of our family was some degree of sick. We can no longer recall who complained of which ailment at any given time, but I do know that I recorded Baker’s first high fever (102.3) on Saturday, 2/24; this was significant because no one else had run a fever up until that point. On 2/25, we opted for a virtual urgent care appointment through the kids’ pediatrician. I just wanted someone to watch Baker breathe–I didn’t like the quickness, the depth of his breaths. Rest assured, the doctor said, his body is working hard, but his breathing isn’t concerning. We were also prescribed Zofran (anti-nausea) just in case Baker’s lack of appetite was due to an upset stomach. So I guess by this point Baker also wasn’t eating. Noted.
Over the next few days, Baker’s fever was relentless. While it would dip back into the range of normal with medicine, it would spike back up the moment it wore off. On Tuesday, 2/27, after recording a fever of 104.4 for the second time, we scheduled an in person urgent care appointment. Once again, face to face this time, Baker’s breathing was assessed and determined to be fine. Baker was diagnosed with an ear infection (the first ever ear infection for our family, believe it or not), and “probably a few other viruses.” We were sent home with antibiotics and the doctor’s reassurance that once the fevers were under control, Baker’s appetite would come back and his breathing would calm down.
On Wednesday, 2/28, despite barely getting any of the antibiotics into the stubborn babe, Baker’s fever only spiked to 101, the lowest it had been all week. On Thursday, 102. We were feeling relatively optimistic on that front! However, it was at this point that Baker stopped breastfeeding. Let’s be clear, Baker LIVES for the boobs. Does he like food? Yes. But would he be fine surviving on boobs and boobs alone? YES. Throughout the entirety of the illness up until this point, Baker was refusing food, but he was still consistently on the breast, so my concerns about his caloric intake were present, but not persistent. Once he stopped breastfeeding… I was worried.
On Thursday evening, I called the nurse line at our pediatrician. At this point, my main concern was hydration, since his main source was now also a no-go. The first nurse I spoke to asked me 100 questions, none of which held much weight in our current issue, and I became increasingly frustrated. When she eventually felt she couldn’t answer my question, she said she would consult the on-call physician and give us a call back. When we finally received a call 4 hours later, I had given up hope that we would actually get a response. The nurse on the phone, someone else this time, assured me that the office was in agreement: unless Baker had zero wet diapers in a 24-hour period, dehydration isn’t a concern.
In the early hours of Friday, 3/1, Baker finally took to my breast for the first time in 2 days. While we still hadn’t managed to get him to keep down any significant portion of his antibiotics, I was overcome with relief when he asked for “milkies.” Morning came, we got out of bed, and Baker immediately vomited the entire contents of his little body, including that milk I had been so grateful for. For the next few hours, we settled into day 7 of our new routine: endless couch snuggles. As Baker continued to fall in and out of sleep on my chest, I watched his breathing and wondered what we could possibly do for him. Zero wet diapers in 24-hours felt insane. For the record, we had our post-discharge follow-up appointment for Baker today and I asked the doctor we saw about the 24-hour time period and she was flabbergasted. She tells her patients 8-hours without a wet diaper is a dehydration concern.
Then I remembered, a dad at our kids preschool is a pediatrician. I reached out, listed Baker’s symptoms, and anxiously awaited a response. Fairly instantly, we were advised to take him to the nearest children’s hospital ER. More for our own reference looking back than anything else, these are the concerns that eventually brought us to the ER: less than 7oz of water and zero food consumed each day for 7 days, relentless fever (102.5 average, 104.4 at its highest) for 7 days, quit breastfeeding for 48+ hours by the time of admission, could not keep down antibiotics as prescribed because he would immediately spit them out, random vomiting seemingly not associated with anything, and this constant, unproductive cough that kept him up at all hours and made it difficult for him to take deep breaths.
At 5pm on Friday, 3/1, my mom came over to watch the big kids and we headed to the nearest children’s hospital. We packed some snacks, a few toys and Baker’s favorite books; we had heard horror stories of 12+ hour stints in the waiting room at this hospital, and we expected to face the same. The triage nurse examined Baker in the lobby for maybe 30 seconds before ushering us into a private triage room. Later we would learn that by her observation, Baker’s lips were blue, a sign of severe oxygen deprivation.
Baker was placed on oxygen as more nurses entered and attempted to take the rest of his vitals. Keeping the oxygen on my screaming baby’s face became my sole purpose. From this point, everything is a bit of a blur. We were only in triage for a few minutes before we were moved into a room in the ER and immediately surrounded by countless nurses and doctors with the utmost concern on their faces. A few words were floated around over and over again… pneumonia, lethargic, and hypoxic (oxygen deficient).

At some point it became very clear that we would not be leaving the hospital any time soon, so we reached out to my parents, who took the big kids back to their house for their first ever sleepover–they were stoked! Luckily, Andrew was in a clear enough headspace to text me important moments so that we would have timestamps to reference later. From his texts, I can paint a decent picture of the next few hours.


At 7:30 pm, an x-ray technician brought a portable machine into our ER room to get scans of Baker’s lungs. While he wasn’t at liberty to give us an official diagnosis, the tech all but confirmed what the doctors suspected: pneumonia. At 7:50 pm, antibiotics were started, which must mean that an IV was placed before then. At 8:30 pm, we were officially admitted to the PICU (Pediatric Intensive Care Unit). At 8:50 pm, the PICU admission team detected a fever and started Baker on medications to treat that as well as an additional antibiotic.

While we had been moved up to the PICU in our ER bed, Baker was given a crib in the PICU. We spent hours trying to get him to settle down and go to sleep, but every time he would doze off he would awaken moments later, confused and afraid, and attempt to rip off all of the wires attached to him. For our memories… He had a BP cuff on one leg, a pulse oximeter on the opposite big toe, 3 leads stuck to his chest to monitor his heart, and an IV in his left hand.

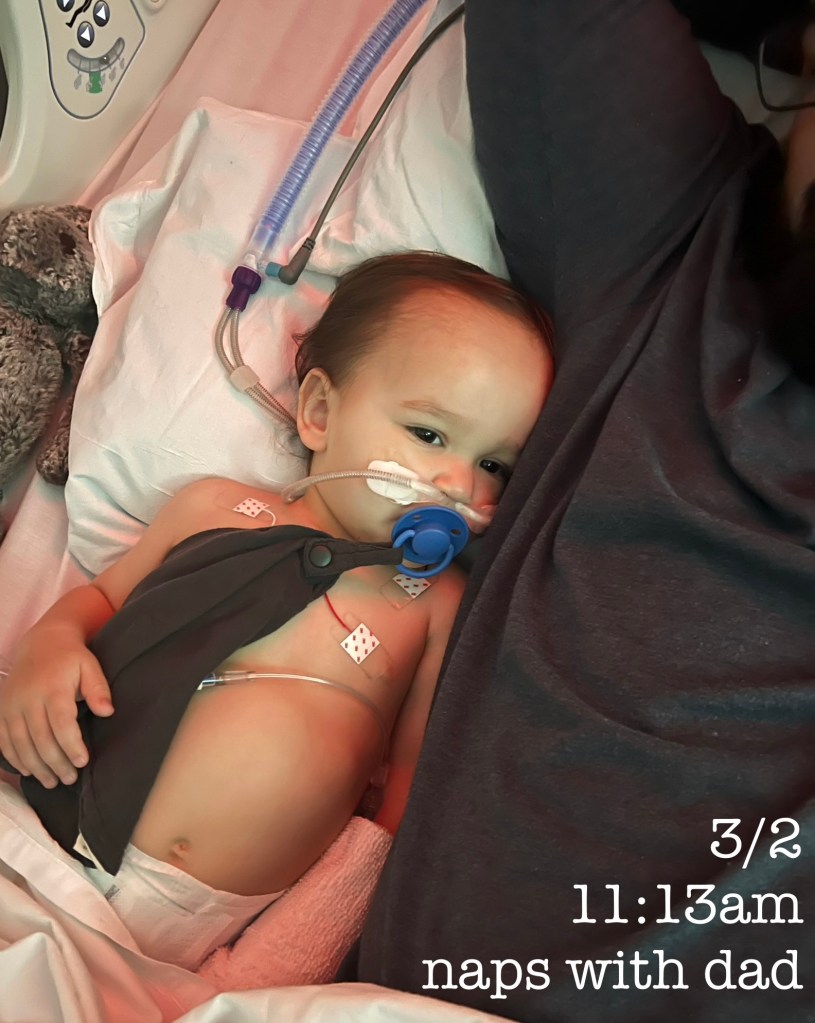
By 11pm, we had accepted our fate, and Baker was asleep in my arms. I was so grateful I could just hold him, though I was warned multiple times that I was not allowed to fall asleep. In the earliest hours of Saturday, 3/2, at 12:30, a new nurse appeared and asked if we would like to swap out the crib for a regular bed so we could sleep with Baker. THANK YOU. I snuggled up next to my sweet boy while Andrew turned the couch in our room into the most uncomfortable, quintessential hospital room bed.
Upon admission to the PICU, Baker’s oxygen had been turned up to its highest point (20L/100%), and we were told he could not receive any nutrients orally for fear of aspiration. This sort of felt like a non-issue at the time because our biggest struggle had been getting him to consume anything; we were grateful for the IV fluids! However, once he could breathe better, Baker’s breastfeeding strike was promptly over, and all he wanted was “milkies.” I lay next to my baby and tried to settle him, but all he wanted was the one thing I couldn’t give him. I had to deny him my breasts whilst he relentlessly signed the baby sign for milk and pleaded with me with his sweet little eyes. I got out of bed and Andrew took my place. I am not a crier, it just isn’t how I process emotions; this is the one time during this whole ordeal that I cried. Denying my sick, helpless baby the thing he could always count on from me… it broke me.

When morning came on Saturday, 3/2, we were exhausted. Nurses came in to check on Baker every hour, and he would randomly wake up and attempt to rip everything off; I listened helplessly from my bed while Andrew soothed him back to sleep over and over again. Throughout the night, they had tested Baker at lower oxygen levels, and by morning, he was on a low enough flow that I was allowed to breastfeed him. This was one of my favorite turning points in his road to recovery… I had missed his sweet little snuggles, his precious little requests for milk. I love him. I love this.

As we settled into our room, we read the “Welcome to the PICU” poster on the wall of our room and learned that the doctors would round at 8:30 am, at which point we assumed we would hear news. Additionally, at some point in the night the white board in our room had been filled out, and under the dianosis section it read, “pneumonia + rhino.” By 10:30 am, however, we hadn’t heard a word. While Andrew went out in search of coffee, I checked my email and noted a bunch of messages from the hospital reading “new test results.” Out of curiousity, I logged into the site and low and behold, Baker’s diagnosis information as well as the findings from his x-rays, none of which had been communicated to us by a human being. I do feel like this was just an oversight, a miscommuncation among staff as we had moved to the PICU so late at night and the ER had been so hectic, but this was the most frustrating part of the whole situation for us I think, having no actual answers as to why our baby was so sick. After reading the information for myself, we buzzed the nurse and she apologetically explained everything we had missed.
Having later read the physicians notes from our hospital stay, Baker’s full diagnosis/reason for admission was: “acute hypoxic respiratory failure secondary to CAP [community-acquired pneumonia, one of the most common acute infections requiring admission to hospital].” His x-ray results read: “Bronchopneumonia with patchy bibasilar airspace disease.” Additionally, upon moving from the ER to the PICU, it was noted, “currently requiring HFNC [high-flow nasal cannula, an oxygen supply system that delivers humidified and heated oxygen at a set flow rate] and still having moderate increased WOB [work of breathing] and tachypnea [abnormally rapid breathing]. Will require close monitoring for worsening status and is at risk for needing intubation.”
Somehow, the whole world didn’t stop when our baby was admitted to the hospital. We still had life and responsibilities, how ridiculous. On Saturday, 3/2, on the first full day of Baker’s hospital stay, I went home to get some things to make the stay more comfortable, while Andrew stayed behind to snuggle our buddy. Our house needed a little TLC since we’d left in such a hurry. I also had 4 dozen cupcakes and 2 layers of a tier cake that I had baked in preperation for a party on Sunday that still needed to be decorated. I spent 5 hours at home, honestly in a bit of a daze. I took a shower and then tried really hard to just focus on decorating the desserts, hoping to give my mind a break from the worry. Unsurprisingly the distraction bit didn’t really work, but I did make some pretty rad mermaid desserts. Let it be known that I would have taken much better and more stylized photos of said desserts had my brain not been elsewhere… I’m a little bummed about that.


I got back to the hospital at around 5pm. I hadn’t missed much, mostly snuggles. On the oxygen front, Baker was continuing to make progress; while he has started the day at 15L/70%, he was down to 7L/30% by 4pm. Baker’s top 2 comfort movies are Ponyo and My Neighbor Totoro, both Studio Ghibli classics, so we settled him in with Ponyo for the evening, and hoped maybe we’d get a bit more rest that night.

After a day of pretty solid strides in oxygen improvement, the decision was made to try to turn it off for the night and see how he would do. Every time he started to struggle, one of the machines in the room would start beeping, and then a nurse would appear. I felt like that happened 100 times, but that’s probably only because it meant I was startled awake each time. Since I could breastfeed again, I was able to sleep in bed with Baker. Ironically, it was while breastfeeding that his stats were the best. Some time in the early hours of the morning, when Baker fell asleep on my boob, the oxygen was off for the longest stint so far. Way to go, boob! And on the note of giving credit to the boob, the IV drip of fluids was also turned off for the night. Since Baker was breastfeeding consistently once again, it became a game of monitoring input/outout to see whether he could maintain hydration sufficiently without IV fluids.

At 8:30 am on Sunday, 3/3, I sent this update to a friend: “We did a trial period off of oxygen during the night but sat was too low so we went back on, tried again this morning and again back on. Refusing to eat or drink much, but we stopped the IV fluids when they ran out in the night to see if that might prompt him to try to eat more. No fever for 12+ hours now!”

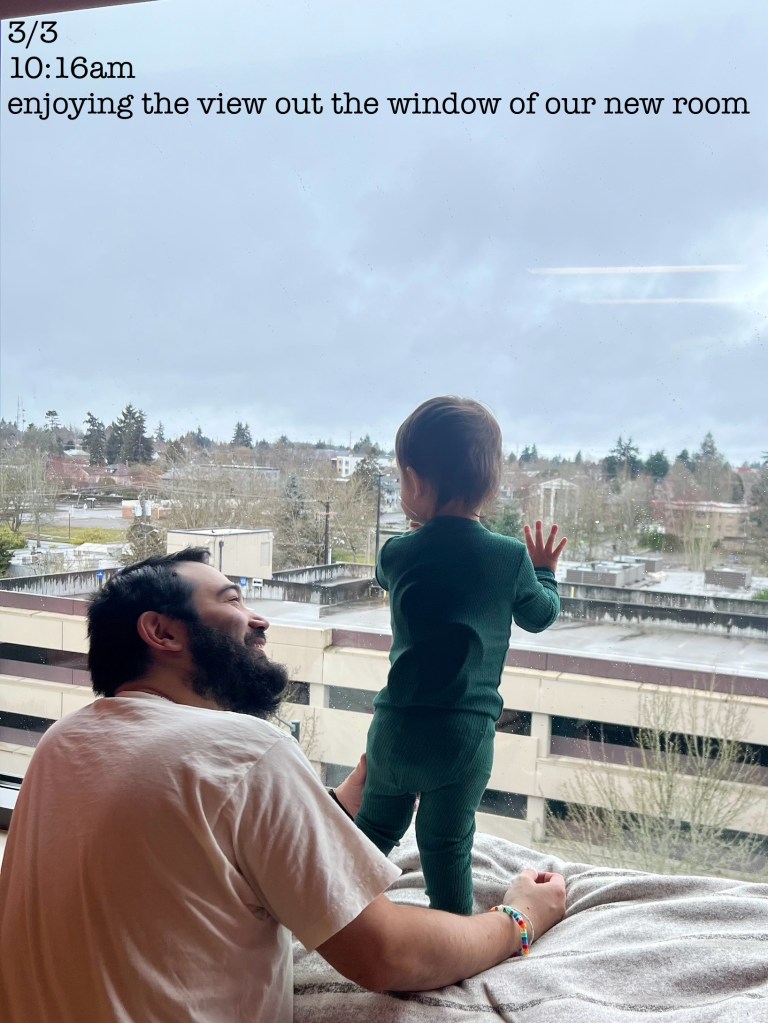
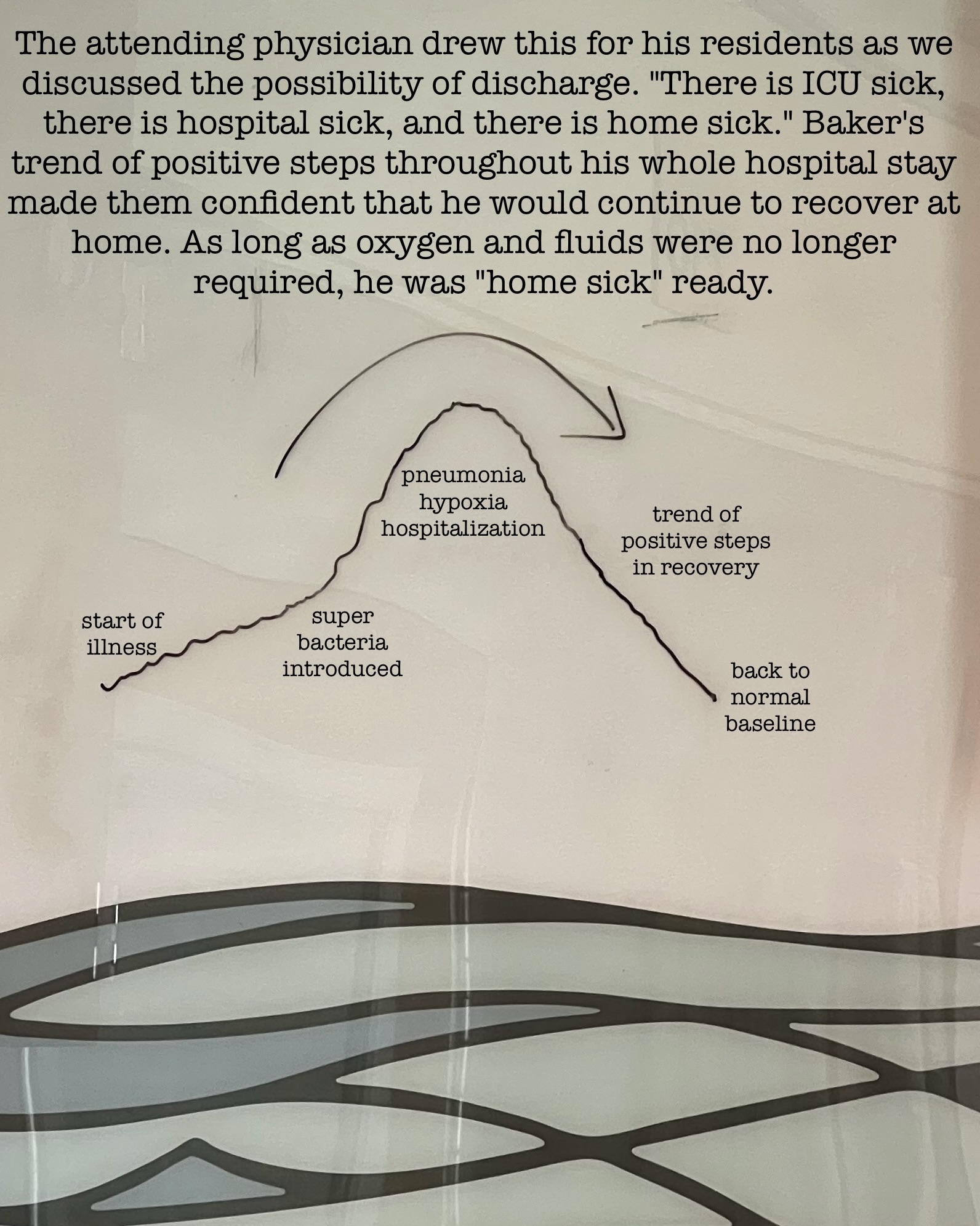
After rounds, the consensus was that while Baker was “still hospital sick, he [was] no longer ICU sick.” With that, we were moved onto the regular pediatric ward. Once we moved over there (which was literally across the hall, by the way… it was so close that Andrew enlisted the help of a nurse to move the rocking chair from our PICU room into our main ward room since it didn’t have one), we tried another stint without oxygen, and we never had to turn it on again.
We started to see a new kid on Sunday. After 24+ hours on antibiotics, fluids and oxygen, Baker was clearly feeling so much better. He actually started to play again, and since he no longer had to be hooked up to half a dozen wires, he was able to move around. We discovered that we could see the tram go by outside, and there was a construction site just within view, two very exciting things for this toddler.

Now that we were out of the PICU and feeling better, it felt like a good time for the big kids to come visit. We were missing them so much. It was really great to see Baker interact with his siblings again, and they definitely brought some more of his personality out.



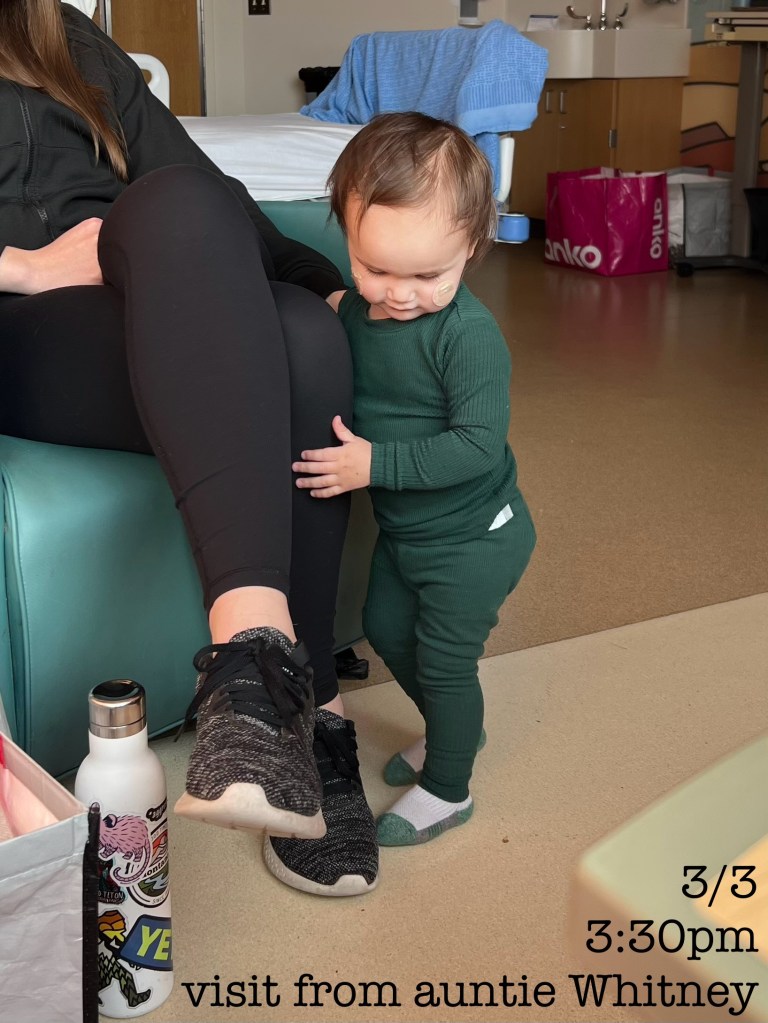
We were popular on Sunday! After my mom left with the kids, my best friend Whitney brought us dinner and some Trader Joes goodies.
At some point that afternoon, we requested Baker’s IV line be removed since it hadn’t been used in 12+ hours and his hand was visibly swollen and uncomfortable. Without the IV, and with permission not to be monitored constantly, I was able to shower with Baker. No more stinky baby! As day 2 in the hospital itched closer into night 3, once again it was abundantly clear that the real world was still happening outside the hospital, and if we wanted any chance of our other kids feeling like they’d have any sort of normal week, Andrew needed to head home to be with them.
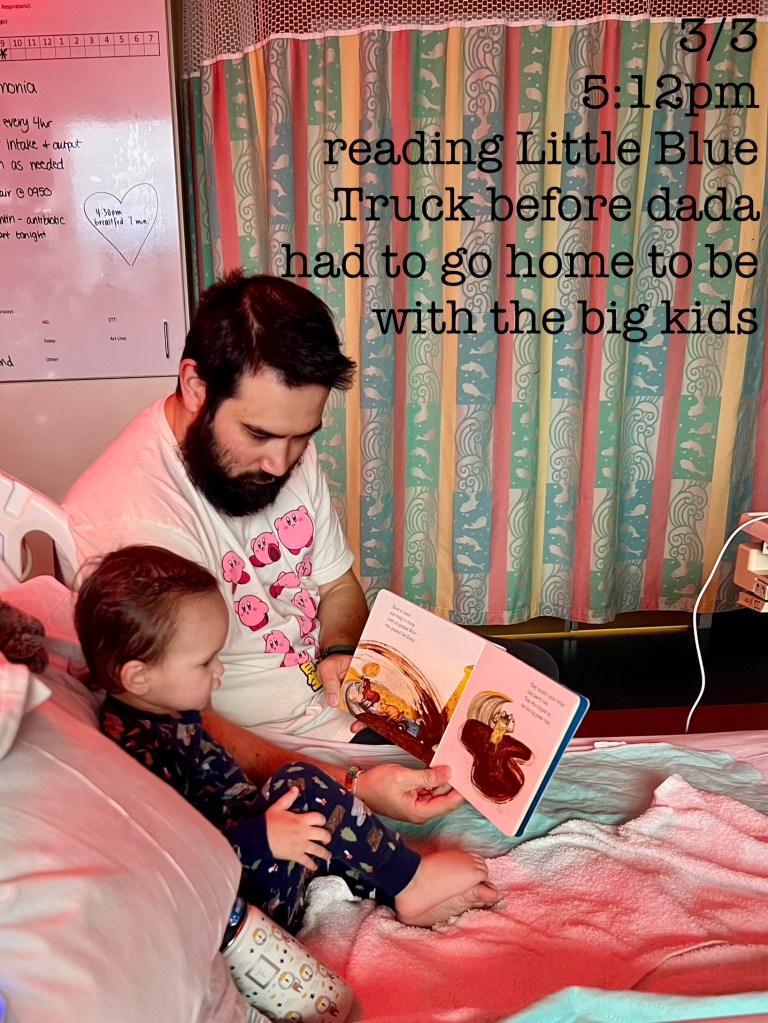
At 5:15 pm, Andrew left, and Baker and I settled in for our first solo night in the hospital. At this point, we were hopeful that discharge was on the horizon… we had been hesitantly told Monday after Baker’s rapid improvement, and we were anxious for that to stick. Not only were we going crazy in the hospital, but I hadn’t packed all that much clothing and we were going to run out if we had to stay much longer.
After Andrew left, the mood shifted a bit for me. Shift change happened at 7pm, and our new nurse was actually a duo! We got a female nurse–as had been the case for the rest of our stay–and with her, a male student! I told Andrew I would try to get a sneaky picture of him… alas, I failed. So you’ll just have to take my word for it. This man was RIPPED. Like, scrubs barely fit ripped. Wait, I was talking about the mood shift… right, okay. The new nurses came on and made it very clear immediately that Baker was on the verge of needing to go back on IV fluids. Although he had been breastfeeding some, he still wasn’t eating or drinking, and he definitely wasn’t breastfeeding enough to make up for the lack of anything else. Desperate not to put him through another IV, I spent the next few hours trying so hard to get Baker to eat.
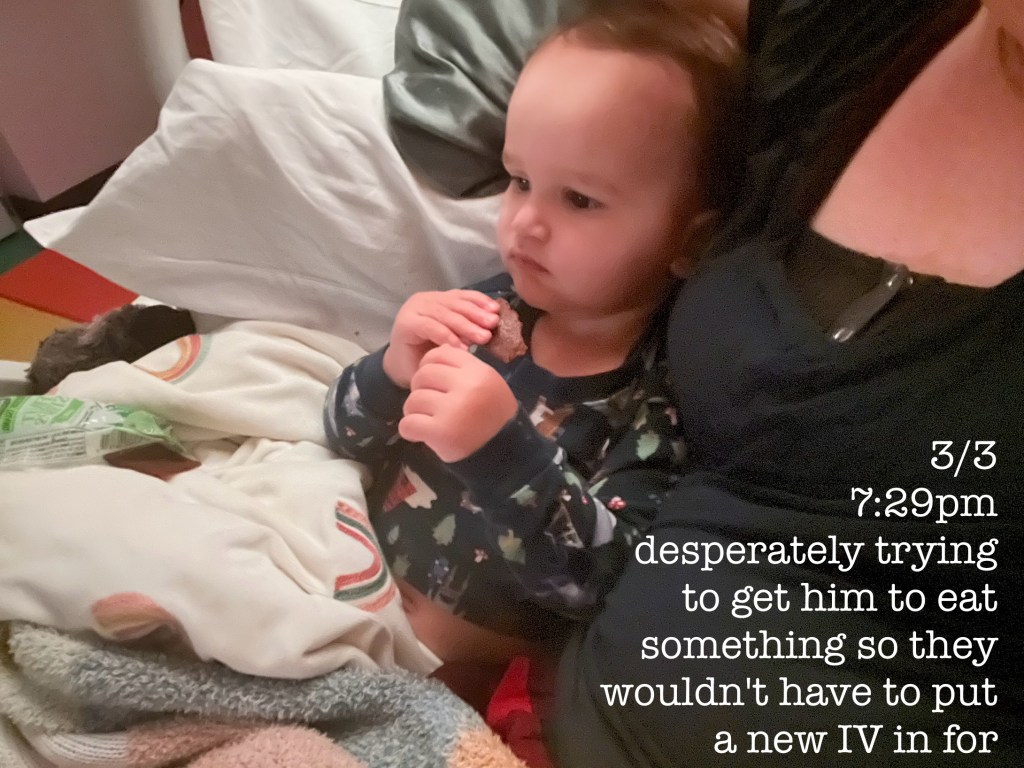
While I managed to get a tiny bit of food in him, I wasn’t feeling particularly optimistic when the nurses arrived to try our first go at oral antibiotics since being admitted. At 8:20 pm, I had managed to get half of the antibiotics down the throat of a baby resisting like we were trying to end his life. I asked the nurses if we could give Baker a break before trying the second half of the meds. They agreed and left the room. The door had barely closed behind them when Baker turned around to look at me and vomited all of our hard work all over the both of us, our bed, our blankets, everything. I paged the nurses back in and handed my screaming, vomit-covered baby to a very apprehensive, very buff man. In what I can only describe as a vomit-covered fugue state, I stood in the shower fully clothed and stripped Baker, scrubbed him head to toe, and handed him back to the nurse so that I could finally remove my own vomit clothes. As I stood in the shower trying not to breathe in the steamy vomit smell while I washed all of our clothes, I really, really missed my husband. He is the vomit parent in our relationship–every relationship has one, right? I needed my vomit man. And a hug.
After the vomit incident, it became clear that IV fluids were inevitable. At 9:10 pm, the IV team came in to place a new line. For 20 minutes, they poked and prodded Baker while he screamed and cried. In the end, they were unsuccessful, so we would have to wait for the most senior nurse to try again. This sought after nurse was apparently out on a transport call, however, so we would have to wait some unknown amount of time before attempting again. After antibiotics forced on him, vomit, vomit speed shower, being thrust upon a very large man, being poked and held down… Baker was exhausted. So was I.

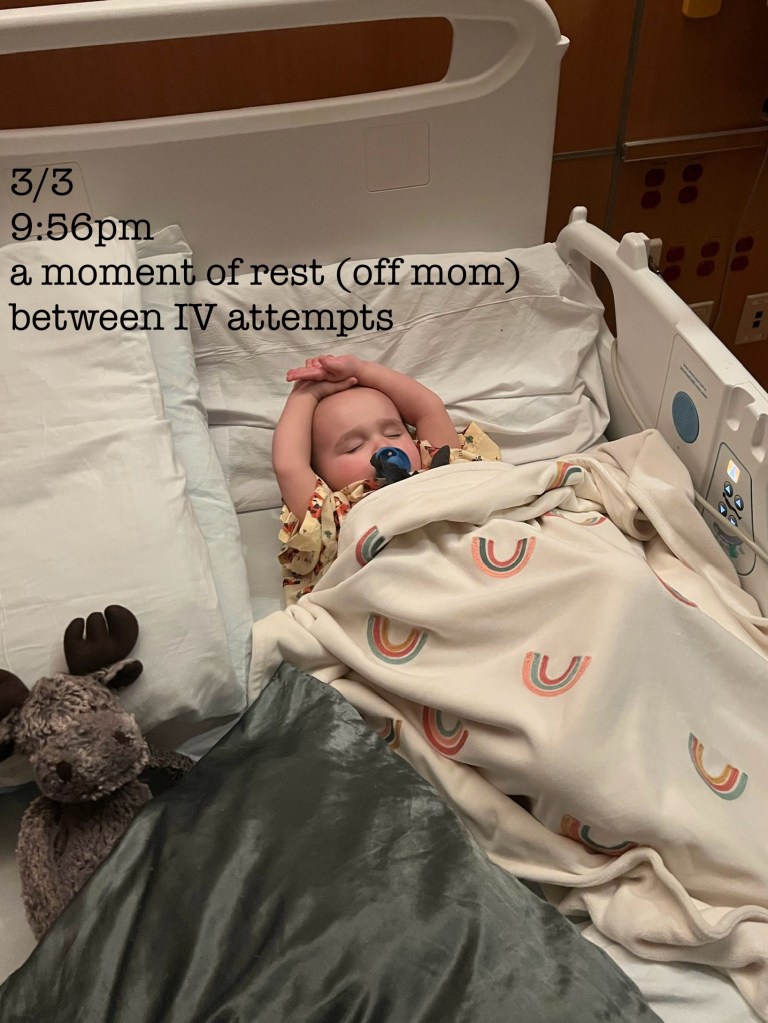
While I was able to settle him alone for a moment, my poor baby just wanted comfort, but I was so wound up after all of the activity of our evening that I wasn’t ready to lay down quite yet. Luckily I still had my carrier with me.
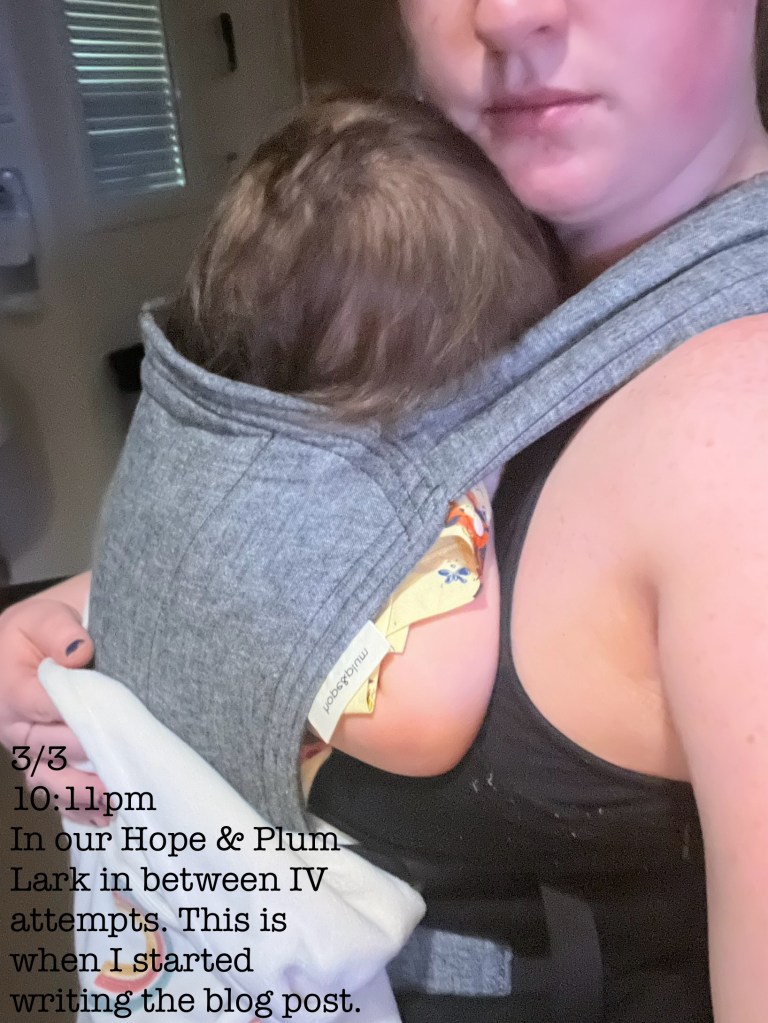
I strapped Baker to my chest, covered him with his remaining blanket that was somehow spared from the vomit, and stood over my computer, hoping maybe I could cope better with words. This is the moment I started writing this post. And while I wasn’t able to get very far into it at that moment, it did help me start to process the trauma of the whole thing.

At 11 pm, the transport nurse returned to the hospital, and we were finally able to start Baker back on IV fluids. I don’t think either of us really recovered from the stress of the evening, so we slept pretty terribly that night on our own. It didn’t help that the nurses had to check on Baker every hour since he was back on the IV, and he’d suddenly decided that boobs were his BFF again, so he asked to breastfeed as often as the nurses came to check on us. The next morning (Monday, 3/4), I was desperate for a real, lengthy shower, and someone else’s arms to hold Baker.

At around 9 am, the IV fluids were turned off, and we got to attempt oral antibiotics once again. By some miracle, Baker took them (not without a fight, but still) and kept them down! Around 9:30, while on FaceTime with Andrew and the kids at home, the doctors came into our room to do rounds for the first time during our stay. Andrew remained on the line as the doctors discussed Baker’s progress, their plan of action, and, to my surprise, moving forward with discharge! Baker would have to remain steady for the next 4 hours or so, keeping down his antibiotics and showing some amount of interest in food, but he was “no longer hospital sick, he could be home sick.”
Shortly after the doctors left, my mom arrived to give me a break. I showered and put on my last clean pair of underwear, so they had better be serious about discharge.

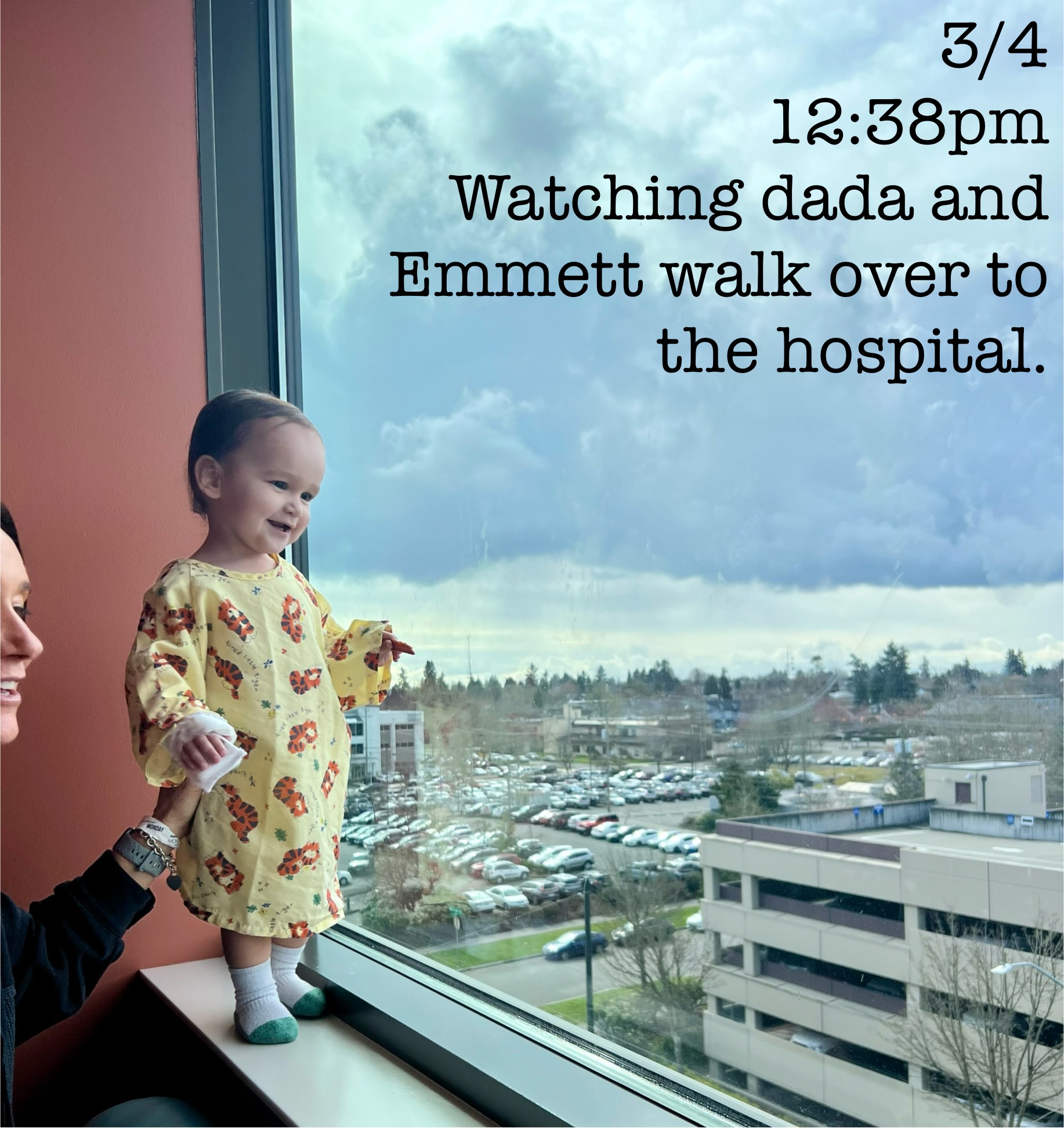
A few hours later, it really felt like our Baker was back. He started to play, like REALLY play. He ran around a little. He eagerly asked to stand in the window, his favorite spot to be whenever possible.



At 12:30, Andrew and Emmett arrived. Our new room overlooked the parking garage across the street, so Andrew parked on the top level and let the boys wave at each other from across the street. They were thrilled!
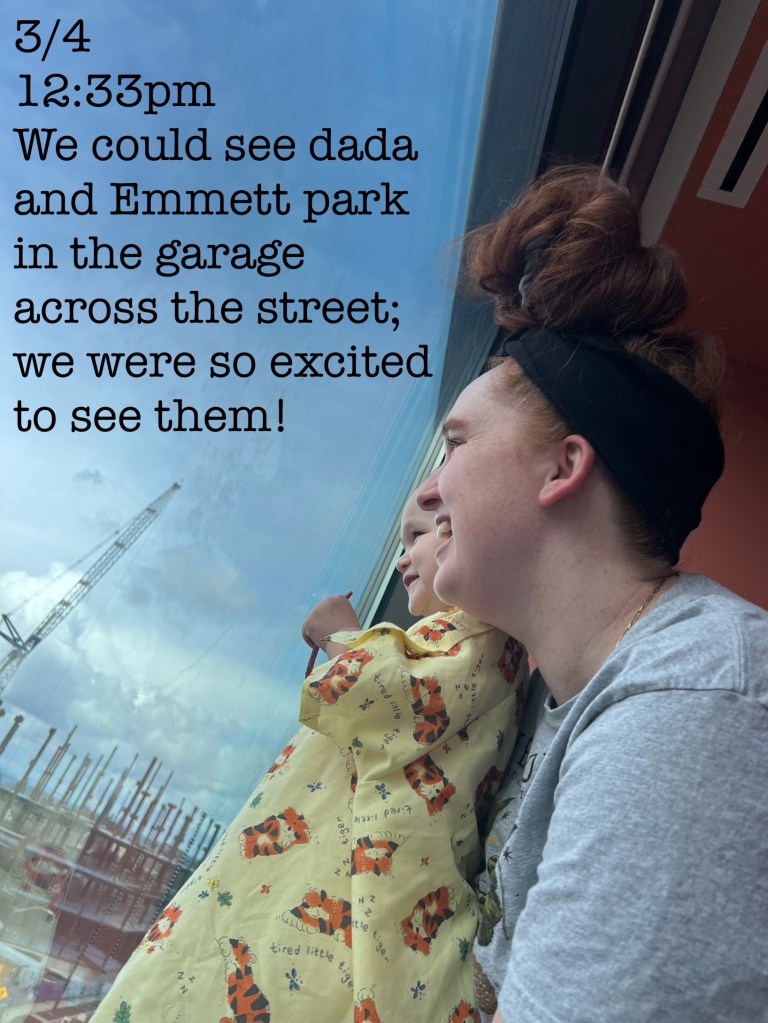

Andrew and I took Emmett on a little date to the hospital cafeteria while my mom stayed with Baker, and then my mom took Emmett home to nap. After the morning’s activities, we’d used up the little energy we had, so Baker and I settled in for a nap, hoping to wake up to discharge orders.

And we did!

At 5:47 pm on Monday, 3/4, I sent this photo to our family with the caption, “WE ARE FREE!!”
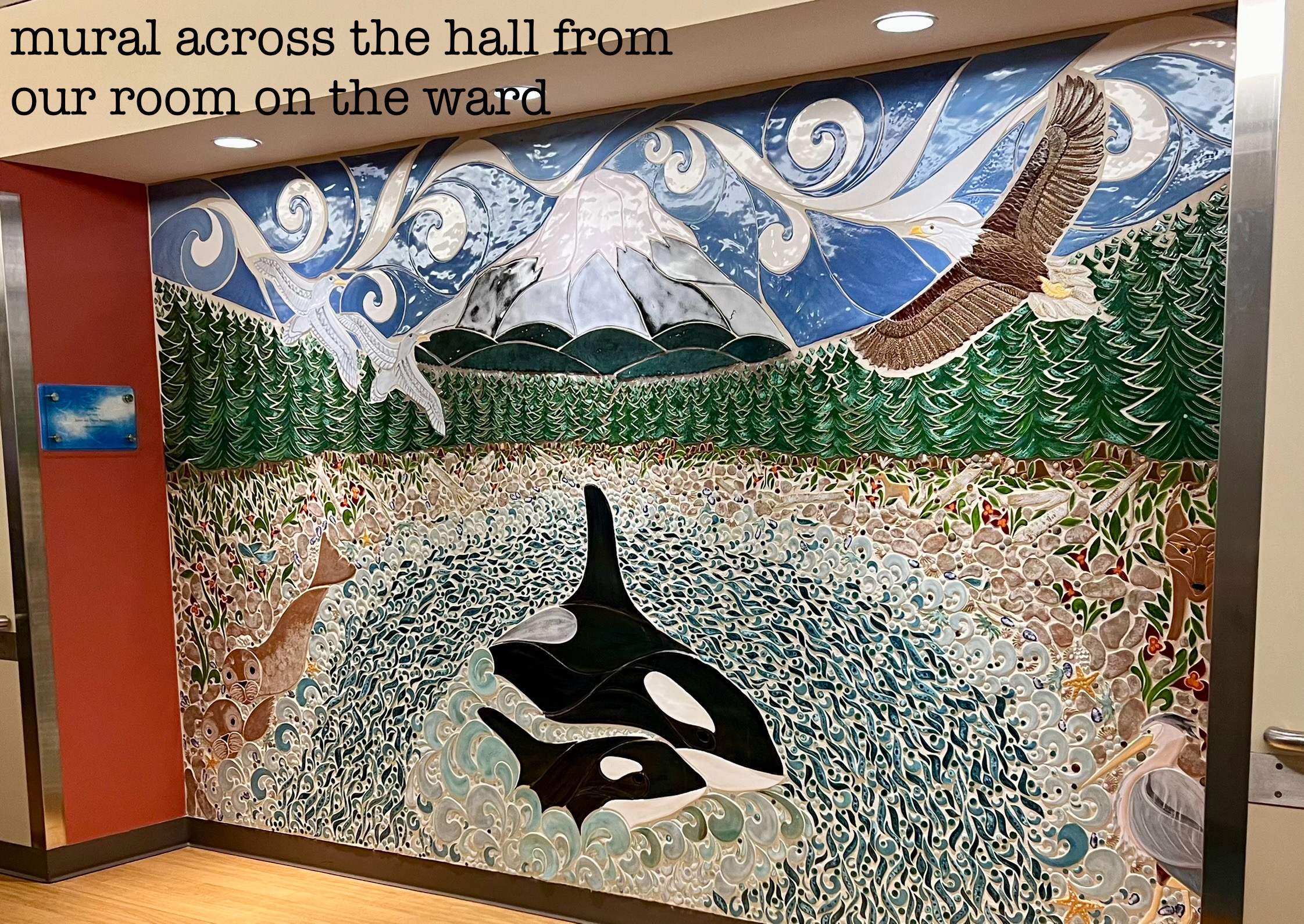
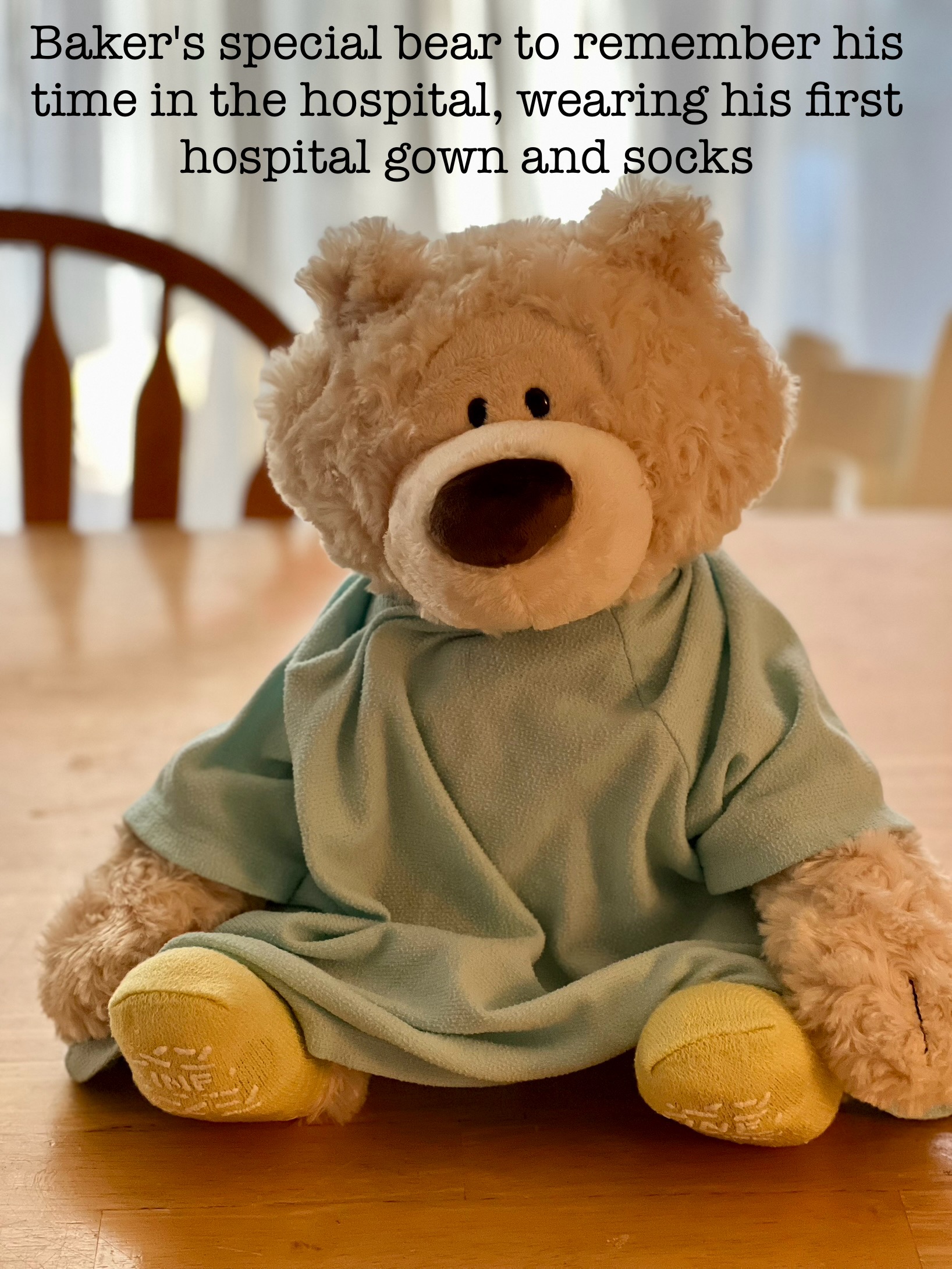
Below are more images from throughout our stay.











This is an entirely unnecessary caveat that I am adding really only for myself in this moment, and for a future moment when I sit down and read this in a more critical light. This is not my best work, this isn’t really even edited. I wrote a whole section of it one night and somehow didn’t save so I had to start over. We’re now a week past discharge as I’m finishing it and it feels like a marathon of a piece. I wanted to get this out there before I forgot, I wanted this memory for me. I hope we never have to go through something like this again, but I also know how lucky we are that Baker recovered so quickly, and that he is doing so well now. So many people are not that lucky. Anyway, this piece wasn’t about the writing, it wasn’t about the style and the format, it was about the memories. So, to future me reading this… give yourself some grace.
